Idioma
Nursing diagnoses, interventions, and outcomes in the immediate postoperative period of cardiac surgery: a scoping review
Nursing diagnoses, interventions, and outcomes in the immediate postoperative period of cardiac surgery: a scoping review
Diagnósticos, intervenções e resultados de enfermagem no pós-operatório imediato de cirurgia cardíaca: revisão de escopo
ABSTRACT
Objective: To identify diagnoses, interventions and/or outcomes, including clinical indicator assessment scales, of patients in the immediate postoperative period of cardiac surgery based on the literature. Method: Scoping review based on the Joanna Briggs Institute manual in 11 research databases or directories. Data analysis identified diagnoses, interventions and outcomes described in standardized and non-standardized language. Results: Of the ten studies included, five contained NANDA International diagnoses. No studies were found that used standardized language for nursing interventions and outcomes, however, one study addressed an intervention with non-standardized language and five studies described clinical nursing indicator scales. Conclusion: This study synthesized the elements of the nursing process for patients in the immediate postoperative period of cardiac surgery based on the literature and can help develop products in this area.
Descriptors: Postoperative Care; Nursing Diagnosis; Perioperative Nursing; Nursing Process; Standardized Nursing Terminology
RESUMO
Objetivo: Identificar diagnósticos, intervenções e/ou resultados, incluindo escalas de avaliação de indicadores clínicos, de pacientes no pós-operatório imediato de cirurgia cardíaca com base na literatura. Método: revisão de escopo baseada no manual do Joanna Briggs Institute em 11 bases ou diretórios de pesquisa. Para a análise dos dados foi realizada a identificação de diagnósticos, intervenções e resultados descritos em linguagem padronizada e em linguagem não padronizada. Resultados: dos dez estudos incluídos, cinco continham diagnósticos da NANDA Internacional. Não foram encontrados estudos que utilizaram linguagem padronizada de intervenções e resultados de enfermagem, no entanto, um estudo abordou uma intervenção com linguagem não padronizada e cinco estudos descreviam escalas de indicadores clínicos de enfermagem. Conclusão: este estudo sintetizou os elementos do processo de enfermagem para pacientes em pós-operatório imediato de cirurgia cardíaca baseados na literatura e pode auxiliar o desenvolvimento de produtos na área.
Descritores: Cuidados Pós-operatórios; Diagnóstico de Enfermagem; Enfermagem Perioperatória; Processo de Enfermagem; Terminologia Padronizada em Enfermagem
INTRODUCTION
Population aging and the disabilities caused by cardiovascular diseases are increasing the demand for surgical correction.1 The surgical approach to the cardiovascular system has recorded a mortality rate of 1.8 to 7.9%, with morbidity between 8.4 and 34.3% in the Society of Thoracic Surgeons' institutions involved in adult cardiac surgery, varying according to the type of procedure.2
In this context, it is necessary to refine cardiology nurses' knowledge of the elements of the Nursing Process (diagnoses, interventions and nursing outcomes), a methodological tool that directs nursing care to achieve improvements in health, for patients undergoing cardiac surgery.3 To replicate and standardize the information recorded by nurses to adapt it to electronic medical records, the documentation of the Nursing Process should be carried out using standardized language systems for its elements.
Standardized language systems help to build evidence, from electronic patient records, of the quality of care and patient safety.4 Considering this, nursing researchers have developed studies to review and validate the elements of the Nursing Process in standardized language systems, as well as qualitative and clinical studies (observational and experimental) to build scientific knowledge in this area.5-8
An integrative review of nursing interventions in the postoperative period of heart surgery identified transitional care and health education as fundamental to reducing complications, hospital readmissions and anxiety. This study highlighted the importance of nursing interventions for post-operative care in cardiac surgery, especially in coronary artery bypass grafting, and the need to expand studies on the subject.9
A prospective longitudinal study of 181 post-operative cardiac surgery patients analyzed the prognostic capacity of the clinical indicators of the nursing diagnosis "Delayed surgical recovery" during hospitalization, observing an incidence of 23.2% of this diagnosis, lasting between 8 and 10 days. The study indicated that the timely recognition of clinical indicators pointing to the nursing diagnosis "Delayed surgical recovery" demonstrates the promising capacity of the diagnosis researched.6
Outlining care through diagnoses, interventions and outcomes in standardized language systems helps organize clinical reasoning for the Nursing Process. Despite this, there are no studies that have identified these elements in the context of the immediate postoperative period of cardiac surgery. In addition, the evaluation of these components in the literature provides support for the development of clinical protocols that highlight the best nursing practices. The Nursing Process, in the context of the immediate postoperative period, includes various problems, actions and results aimed at recovery from anesthesia, prevention of complications and comfort. Therefore, this review is justified because it presents this field of research interest in its entirety.10
OBJECTIVE
To identify nursing diagnoses, interventions and/or outcomes, including clinical indicator assessment scales, for patients in the immediate postoperative period of cardiac surgery, based on the literature.
METHOD
This is a scoping review study based on the Joanna Briggs Institute manual and guided by the Preferred Reporting Items for Systematic reviews and Meta-Analyses Extension for Scoping Reviews (PRISMA-ScR).10-11 The review was registered on the Figshare and Open Science Framework platforms.12-13.
The research question was guided by the acronym PCC (Population, Concept and Context)10: Population - adult patients undergoing cardiac surgery with sternotomy; Concept - nursing diagnoses, interventions, and outcomes; and Context - period of the POI.
Therefore, the research question was: what nursing diagnoses, interventions and outcomes are present in nursing care for adult patients in the immediate postoperative period of cardiac surgery?
The sources of evidence were experimental and quasi-experimental studies, including randomized or non-randomized controlled studies, time series, descriptive observational study designs, before and after studies, cross-sectional analytical studies, such as case series, analytical observational studies, prospective and retrospective cohort studies, case-control studies, individual case reports and descriptive cross-sectional studies. Qualitative studies were also considered. Editorials, letters to the editor, opinion pieces and reviews were excluded. No specifications were set regarding the year of publication or language, but only completed studies were included. Studies that addressed the concepts of interest to the research were considered, even if they included applications referring to other perioperative periods.
Before starting the study, a search was carried out in April 2021 in the PROS-PERO, Medical Literature Analysis and Retrieval System Online - PubMed (MEDLINE - PubMed), Cochrane and Joanna Briggs Institute databases, and no reviews in progress or finalized on this topic in the last two years were identified.
The identification stage began with a preliminary search of similar publications in the literature for terms in the titles, abstracts and descriptors related to PCC, which led to the search for controlled vocabulary: Health Sciences Descriptors (DeCS) from the Virtual Health Library (VHL), Medical Subject Headings (MeSH) from Pub-Med and Embase Subject Headings (Emtree) from Embase.
A full secondary search with controlled and non-controlled words, along with the delimiting operators (AND, OR and the NOT operator was not used), was carried out in April 2021, with the search being updated in March 2023 in the following databases: VHL, Cochrane Library, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Epistemonikos, Embase, National Institute for Health and Clinical Excellence, PubMed Central, PubMed, Scientifc electronic library online (Scielo), Science. gov, Scopus and Web of Science (WoS). In the identification stage, the search strategy was defined by relating all the PCC terms according to the search configuration of each database. The search strategies are available in the scoping protocol registered on the Figshare and Open Science Framework platforms. 12-13
A third search strategy involved evaluating the main references of the studies surveyed and searching the gray literature in the thesis and dissertation repositories of universities with study groups focused on cardiac surgery.
Once the searches had been carried out, the titles and abstracts were read, and the studies were grouped as follows: 1 - Included for full reading, 2 - Excluded for not fitting the Population, 3 - Excluded for not fitting the Concept, 4 - Excluded for not fitting the Context and 5 - Excluded for not fitting the PCC (when they did not fit more than one of the PCC items). The abstracts and full texts were read blindly by two researchers, and any discrepancies were resolved by reading the full study together and discussing it.
In the inclusion stage, the studies were categorized as: 1 - Included for the extraction phase, 2 - Excluded due to unavailability of the full text, 3 - Excluded due to duplicate text (same study published in different languages) or 4 - Excluded due to not describing nursing diagnoses, interventions, or outcomes.
The results were synthesized in the following stages: 1 - Identified studies with nursing diagnoses in the standardized language of the NANDA-International (NANDA-I)15; 2 - Identified studies with nursing diagnoses in non-standardized language; 3 - Identified studies with nursing interventions in the standardized language of the Nursing Intervention Classification (NIC)16; 4 - Identified studies with nursing interventions in non-standardized language; 5 - Identified studies with nursing outcomes in standardized language from the Nursing Outcomes Classification (NOC)17; 6 - Identified studies with nursing outcomes in non-standardized language; 7 - Identified studies that described scales of clinical nursing indicators.
In each study included, the data was categorized according to the following items: journal of publication; author, year of publication; research design; and sample size and phenomenon identified (nursing diagnoses, nursing interventions, nursing outcomes, clinical indicator scales and standardized language system).10,14. The data was extracted from the studies by two researchers, in a shared way, using Google Drive spreadsheets.
RESULTS
After removing duplicates, the search identified 1,897 studies. At the end of the selection process, ten studies were included. The PRISMA-ScR18 flowchart shows the process of selection and final inclusion of the studies, and at the end shows the total number of biographical searches carried out (Figure 1).
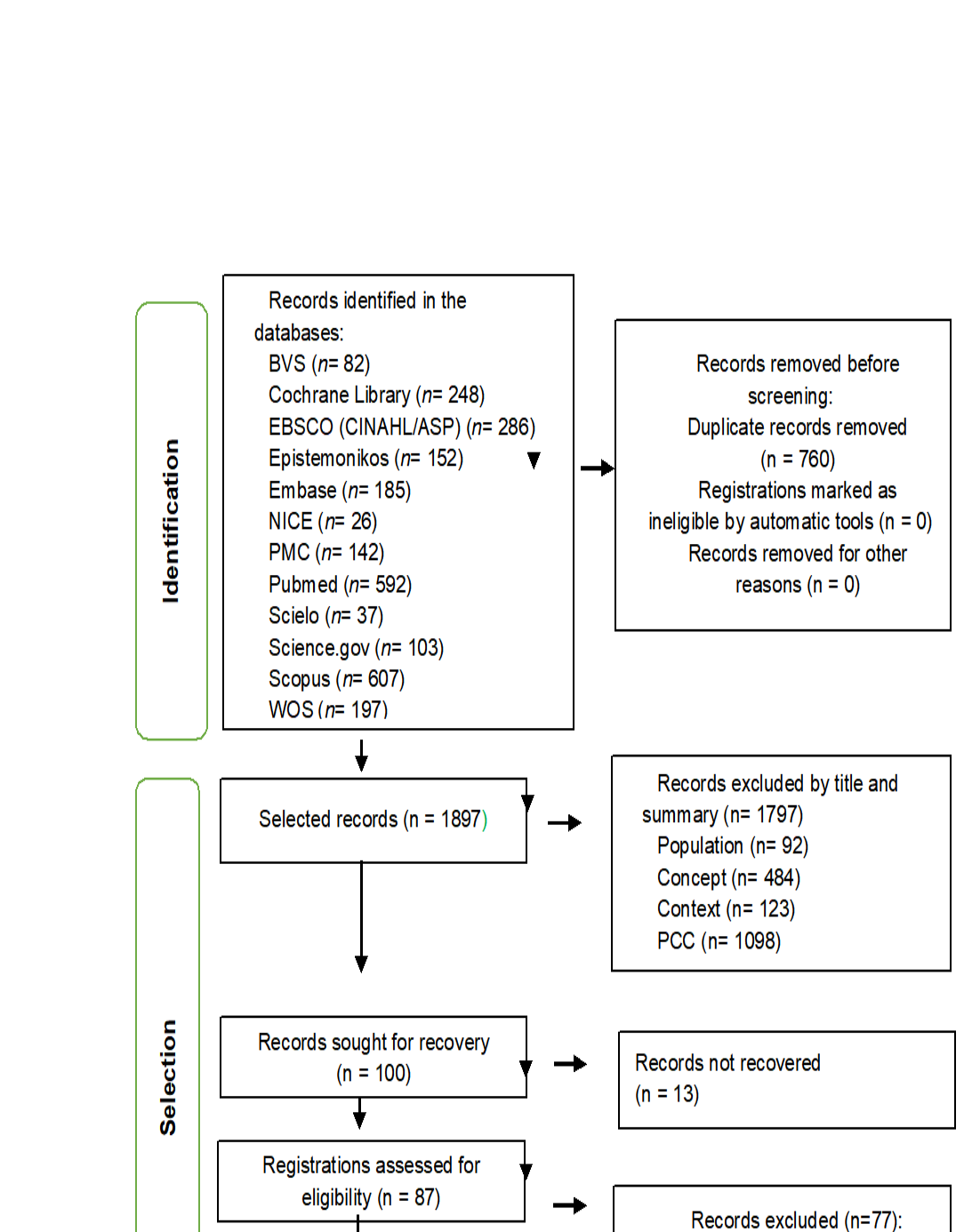
Figure 1 - PRISMA flowchart of the scope review. Niterói, RJ, Brazil, 2023
Table 1 shows the characterization of the ten studies according to journal, first author, year of publication, research design, sample and phenomenon identified.
Table 1 - Characterization of the studies included in the scoping review. Niterói, RJ, Brazil, 2023.
|
Journal / author/year |
Method/ No |
Phenomenon |
|
Rev Esc Enferm USP Galdeano et al.19 2006 |
Descriptive observational n=17 |
Nursing diagnoses (NANDA-I) = 11 Pain, Risk of Infection, Risk of Perioperative Positioning Injury, Risk of Peripheral Neurovascular Dysfunction, Risk of Aspiration, Impaired Skin Integrity, Sensory/Perception Changes, Impaired Verbal Communication, Ineffective Airway Clearance, Impaired Physical Mobility and Altered Protection.
|
|
Nurs Crit Care Feuchtinger et al20 2007 |
Prospective exploratory n=53 |
Nursing score (clinical scale) = 1 Braden Scale: a scale that assesses the risk of developing a pressure injury. The study indicates that the Braden scale should not be used for cardiac surgery patients in the first five days after the surgical procedure.
|
|
Ann Thorac Surg Bickert et al21 2008 |
Prospective n=315 |
Nursing score (clinical scale) = 1 Neurologic Intensive Care Evaluation (NICE): scale for evaluating neurological status by screening for delirium
|
|
Pain Manag Nurs Marmo et al22 2010 |
Observational descriptive series n=25 |
Nursing results (clinical scale) = 2 Critical-Care Pain Observation Tool (CPOT): scale that assesses the presence of pain in patients with an advanced airway or not Non-Verbal Pain Scale (NVPS): scale for quantifying pain in patients unable to verbalize
|
|
Rev Latino-Am Enfermagem Guimarães et al23 2010 |
Prospective cohort n=55 |
Nursing outcome (clinical score) = 1 TISS-28 score that measures the workload of nursing staff in intensive care units and estimates the severity of patients.
|
|
AJCC Exarchopoulos et al24 2015 |
Prospective cohort n=150 |
Nursing outcome (clinical score) = 1 EuroSCORE II: score for assessing surgical risk and predicting the outcome of cardiac surgery patients. |
|
REUFSM Fontes de Lara et al25 2017 |
Cross-section n=50 |
Nursing diagnoses (NANDA-I) = 11 Decreased Cardiac Output, Risk of Impaired Fluid Volume, Risk of Infection, Impaired Tissue Integrity, Impaired Verbal Communication, Risk of Impaired Skin Integrity, Impaired Physical Mobility, Risk of Fall, Risk of Aspiration, Hypothermia, Interrupted Family Processes.
|
|
Eur J Cardiovasc Nurs Santos et al26 2017 |
Prospective cohort n=257 |
Nursing diagnosis (NANDA-I) = 1 Decreased cardiac output Non-standardized language nursing intervention = 1 Monitor heart rate and rhythm for at least 48–72 hours.
|
|
SOBECC Andrade et al5 2019 |
Observational n=50 |
Nursing diagnoses (NANDA-I) = 16 Decreased Cardiac Output, Risk of Bleeding, Risk of Decreased Cardiac Tissue Perfusion; Risk of Shock, Acute Pain, Risk of Infection, Risk of Unstable Blood Sugar, Risk of Fall, Impaired Skin Integrity, Ineffective Respiratory Pattern, Ineffective Peripheral Tissue Perfusion, Impaired Physical Mobility, Deficit in Self-Care for Bathing, Anxiety, Risk of Constipation, Unbalanced Nutrition: Less than Body Needs.
|
|
J Nurs Scholarsh Gomes do Carmo et al6 2021 |
Prospective cohort n=181 |
Nursing diagnosis (NANDA-I) = 1 Delayed Surgical Recovery |
Five studies were identified with nursing diagnoses (50%)5-6,19,25-26, one with nursing intervention (10%)26 and five with nursing outcomes (50%)20-24.
Of the five studies with nursing diagnoses5-6,19,25-26, four (80%) used the NANDA-I standardized language system5-6,19,26 and one (20%) did not report using standardized language25. Although this study did not use standardized language, it was observed that all the titles of nursing diagnoses identified in it were exact matches to those found in NANDA-I15. Thus, all five studies in which nursing diagnoses were identified were considered to use standardized language.
A total of 29 NANDA-I nursing diagnoses were identified in the five studies5-6,19,25-26 that dealt with diagnoses. All the diagnosis titles were mapped to their corresponding version in the 2021-2023 version of NANDA-I15. One diagnosis was excluded because it was discontinued from the classification. Thus, the final sample consisted of 28 identified nursing diagnoses. The nursing diagnoses identified, stratified according to the frequency with which they appeared in the studies, are shown in Table 2.
Table 2 - Nursing diagnoses identified in the scoping review. Niterói, RJ, Brazil, 2023.
|
Nursing diagnosis (diagnosis code) |
N (%) |
|
Decreased cardiac output (00029) |
3 (60%) |
|
Impaired physical mobility (00085) |
3 (60%) |
|
Risk for infection (00004) |
3 (60%) |
|
Impaired verbal communication (00051) |
2 (40%) |
|
Acute pain (00132) |
2 (40%) |
|
Impaired skin integrity (00046) |
2 (40%) |
|
Risk for falls in adults (00303) |
2 (40%) |
|
Risk for aspiration (00039) |
2 (40%) |
|
Anxiety (00146) |
1 (20%) |
|
Bathing self-care deficit (00108) |
1 (20%) |
|
Ineffective airway clearance (00031) |
1 (20%) |
|
Hypothermia (00006) |
1 (20%) |
|
Impaired tissue integrity (00044) |
1 (20%) |
|
Imbalanced nutrition: less than body requirements (00002) |
1 (20%) |
|
Ineffective breathing pattern (00032) |
1 (20%) |
|
Ineffective peripheral tissue perfusion (00204) |
1 (20%) |
|
Interrupted family processes (00060) |
1 (20%) |
|
Ineffective protection (00043) |
1 (20%) |
|
Delayed surgical recovery (00100) |
1 (20%) |
|
Risk for shock (00205) |
1 (20%) |
|
Risk for constipation (00015) |
1 (20%) |
|
Risk for unstable blood glucose level (00179) |
1 (20%) |
|
Risk for impaired skin integrity (00047) |
1 (20%) |
|
Risk for decreased cardiac tissue perfusion (00200) |
1 (20%) |
|
Risk for bleeding (00206) |
1 (20%) |
|
Risk for peripheral neurovascular dysfunction (00086) |
1 (20%) |
|
Risk for perioperative positioning injury (00087) |
1 (20%) |
|
Deficient fluid volume (00027) |
1 (20%) |
Among the 28 nursing diagnoses identified, the most frequently found were "Decreased cardiac output" (00029)5,25-26 (n=3; 60%), "Impaired physical mobility" (00085)5,19,25 (n=3; 60%) and "Risk of infection" (00004)5,19,25 (n=3; 60%).
No studies were identified with standardized language nursing interventions, and only one study cited a nursing activity ("Monitor heart rate and rhythm") to monitor arrhythmias in adults undergoing cardiac surgery.26
No studies were identified with nursing outcomes in standardized or non-standardized language. Five studies20-24 with clinical nursing indicator scales were identified. Two pain assessment scales were identified, the Care Pain Observation Tool (CPOT) and the Nonverbal Pain Scale (NVPS)22. A neurological assessment scale, the Neurologic Intensive Care Evaluation (NICE)21, a score for predicting patient outcomes, the European System for Cardiac Operative Risk Evaluation (EuroS-CORE II)24, and a score for measuring the severity of intensive care unit (ICU) patients or nursing workload, the Therapeutic Intervention Scoring System-28 (TISS-28)23.
DISCUSSION
This study identified 28 standardized language nursing diagnoses5-6,19,25-26, one non-standardized language nursing intervention26 and five non-standardized language nursing outcomes20-24 to guide the nursing process in the immediate postoperative period of cardiac surgery.
Nursing diagnoses for patients in the immediate postoperative period of cardiac surgery have been studied; however, more studies are needed on standardized language nursing interventions, which are effective and can have an impact on improving diagnoses for these patients. Scales are cited in studies on nursing outcomes, although NOC is not.17
Regarding nursing diagnoses, it was observed that the NANDA-I standardized language system15 was present in all the studies that presented diagnoses, which are widely used. Even so, there are better results in the quality of the advanced nursing process when the NANDA-I classification is used.27 In this context, the most frequently cited nursing diagnoses in this study were: decreased cardiac output, risk of infection and impaired physical mobility.
The diagnosis "Decreased cardiac output", defined as an inadequate volume of blood pumped by the heart to meet metabolic needs,15 was present in 60% of the sample of studies with diagnoses in this review. This diagnosis is frequently observed in the immediate postoperative period of cardiac surgery.5,25-26,28-29
Low cardiac output syndrome is usually the result of left ventricular dysfunction and decreased stroke volume, which may be due to decreased preload, increased afterload, or decreased contractility. Post-cardiac surgery patients can develop low cardiac output syndrome transiently in the first six to eight hours due to myocardial ischemia and reperfusion lesions secondary to cardioplegic arrest.30
In the postoperative period of cardiac surgery, the nursing team should monitor for signs and symptoms of changes in the patient's cardiac output.30 Inadequate myocardial protection, associated with the patient's condition and numerous perioperative factors, including prolonged aortic clamping time and myocardial ischemia, can contribute to the development of low cardiac output syndrome.31
A retrospective observational cross-sectional study that captured data from 59,810 post-cardiac surgery patients recorded the presence of low cardiac output syndrome in 6,067 patients (10.1%). In this study, it was observed that in-hospital mortality was 12 times higher in patients who developed low cardiac output syndrome, as well as an increase in the length of ICU stay and hospital readmission of up to 30 days.32 Low cardiac output in the postoperative period of heart surgery is associated with a higher risk of needing renal replacement therapy and multiple organ failure.33-34
Infections are also an incident complication in the postoperative period of cardiac surgery, corroborating the presence of the nursing diagnosis "Risk of infection", which occurs in individuals susceptible to the invasion of pathogenic microorganisms with the potential to compromise their health.15
Deep sternal infection is observed in 0.2 to 0.6% of postoperative patients, varying according to the cardiac surgical procedure.35 Among open-heart surgery patients, there is a 20.3% incidence of postoperative infection, the most common being pneumonia (9.1%), surgical site infection (7.3%), urinary tract infection (5.3%), bloodstream infection (2.7%), endocarditis (0.5%) and enterocolitis caused by Clostridium difficile (0.3%).36
"Decreased cardiac output" and "Risk of infection" are diagnostic situations for nurses and influence the prognosis and severity of the cardiac patient. Early diagnosis, prevention and treatment of these situations are crucial for post-cardiac surgery patients who develop these complications.30
The nursing diagnosis "Impaired physical mobility", defined by the presence of a limitation in the ability to move the body or extremities independently and voluntarily15, was one of the three most common diagnoses in the immediate postoperative period of cardiac surgery. Mobility problems affect 36.9% of individuals undergoing open-heart surgery.37
Studies indicate that coronary heart disease is often related to the diagnosis "impaired physical mobility". This diagnosis is present in 33.3% of coronary heart disease patients in the period before the intervention.38 Among patients with acute myocardial infarction, the presence of the diagnosis "Impaired physical mobility" reaches 70%.39
However, although it is a nursing diagnosis frequently observed in patients with coronary heart disease, nursing interventions aimed at altering "impaired physical mobility" in patients in the immediate postoperative period of cardiac surgery, a period in which the patient is still in the ICU under surveillance for signs of pregnancy, may not influence recovering the patient's mobility.
Evidence is insufficient to determine the effects of early intervention with early mobilization or active exercise provided to critically ill adults. It is not possible to determine whether early movement or exercise in critically ill people improves their ability to do daily activities, muscle strength or quality of life.40 The lack of evidence of the effectiveness of interventions to modify the impairment of the patient's mobility in the critically ill may explain the absence of nursing interventions for this diagnosis in this scoping review.
In fact, no standardized language nursing interventions were identified in this scoping review. Only one study cited the activity of ″Monitoring heart rate and rhythm for at least 48-72 hours‶ to modify the diagnosis ″Decreased cardiac output‶.26 The activity of ″Monitoring heart rate and rhythm‶ is part of the NIC intervention entitled ″Monitoring Vital Signs‶ (6680). 16 The nursing intervention ″Monitoring Vital Signs‶ was present in 79.4% of the nursing prescriptions for patients with decompensated heart failure analyzed in a descriptive exploratory study.41
There are many other NIC16 nursing interventions that can be prescribed by nurses to modify the main nursing diagnoses in the immediate postoperative period of cardiac surgery, but these are described in the studies. In addition to "Vital signs monitoring", the intervention "Cardiac care: acute phase" (4044) can also be prescribed to change the diagnosis "Decreased cardiac output". For the diagnosis "Risk of infection", the intervention "Protection against infection" (6550) is useful.16 For the diagnosis "Impaired physical mobility", as already mentioned, prescriptions aimed at promoting activity in the immediate postoperative period of cardiac surgery are not appropriate.
Clinical assessment scales were included in this review because they provide a strong basis for diagnostic decision-making and the evolution of nursing outcomes. The scales identified in the context of post-cardiac surgery were aimed at pain stratification in sedated patients (CPTO and NVPS)22, neurological assessment (NICE)21, prediction of clinical outcomes (EuroSCORE II)24 and measurement of ICU patient severity or nursing workload (TISS-28)23. A result was also identified showing that the routine assessment of patients in the immediate postoperative period of cardiac surgery for the risk of developing pressure injuries using the Braden scale should be dispensed with.20
Two pain assessment scales were identified in the scoping review (CPTO and NVPS)22 and only the CPOT is cross-culturally validated in Brazil. The CPOT scale, validated in several countries with cardiac surgical patients, stratifies pain in non-comatose and delirious patients who are unable to report pain reliably.42 The NVPS scale, although its psychometric properties have been validated43, there are still no studies on its scale validation in Brazil. The CPOT remains one of the tools with the strongest psychometric properties for critically ill and sedated patients.44
The NICE scale assesses the neurological condition, is simple to apply and highly reliable because it does not depend on the patient's verbalization and does not interfere with the performance of nursing activities.45 This scale identifies patients at risk of adverse events due to neurological alterations at an early stage.21
EuroSCORE II24, whose purpose is to measure the clinical outcome of cardiac surgical patients, estimates mortality in the postoperative period of cardiac surgery and is available in the form of an electronic calculator with free online access. Although the score's calibration and discrimination are questioned when evaluating specific surgical groups, EuroSCORE II is widely used and is still considered the best predictor of mortality in cardiac surgery.46-47 Another instrument, the TISS-28 score,23 is a practical system for measuring patient severity and ICU nursing workload that compares data between intensive care units in different institutions.48
Postoperative management includes frequent monitoring of vital signs and continuous vigilance for any signs of complications that may arise.30 From this perspective, the profile of the measurement scales described is congruent with the findings regarding the most prevalent nursing diagnoses in the review.
Although these scales are valid for measuring the presence or absence of certain nursing diagnoses in the immediate postoperative period of cardiac surgery, there are NOC17 nursing outcomes that could be used for this same measurement, and which could monitor the effectiveness of the interventions prescribed for each diagnosis identified. Examples of NOC nursing outcomes that could be used in the immediate postoperative period of cardiac surgery are: "Vital signs" (0802) and "Cardiac pump efficacy" (0400) for the diagnosis "Decreased cardiac output" and "Respiratory status: Airway permeability" (0410) for the diagnosis "Risk of infection".17
The prevalence of studies describing diagnoses and the lack of studies describing nursing interventions and outcomes for the immediate postoperative period of cardiac surgery reveals an important deficit in the literature that may be interfering with the clinical reasoning process for the Nursing Process. The nursing diagnosis is the basis for planned interventions and achieving results, but the lack of studies of nursing interventions and results for the immediate postoperative period of cardiac surgery based on standardized language systems demonstrates the lack of interconnection between the stages of the Nursing Process.
More studies of nursing interventions are needed, describing interventions aimed at the NANDA-I15 diagnoses in the immediate postoperative period of cardiac surgery. There is also a need for studies relating the NOC17 nursing outcomes to the NANDA-I15 diagnoses and to the scales presented for the immediate postoperative period of cardiac surgery.
Limitations of the study
One of the limitations of this study was that it only considered standardized language from the NANDA-I, NIC and NOC classifications. Another limitation to be mentioned is that the search in the gray literature was carried out only in the repositories of theses and dissertations from universities with study groups focused on cardiac surgery, without including other sources such as abstracts published in event proceedings, books, and others.
CONCLUSION
This study synthesized the elements of the Nursing Process for post-cardiac surgery patients by identifying 28 nursing diagnoses in standardized language and five scales of clinical nursing indicators for such patients. No standardized language nursing interventions or outcomes were identified.
The main ND identified were: Decreased Cardiac Output, Risk of Infection, and Impaired Physical Mobility. The scales identified were Care Pain Observation Tool, Nonverbal Pain Scale, Neurologic Intensive Care Evaluation, EuroSCORE II and TISS-28 score.
The elements synthesized can contribute to nursing by providing data for documenting the nursing process in post-cardiac surgery ICUs, supporting the development of products, the transfer and implementation of techniques and technologies with the potential to impact health outcomes.
It also contributes to care practice, teaching, and research. For practice, it provides information for judgment and clinical decision-making, favoring patient safety and quality of care by reducing adverse events. The study also provides evidence for teaching the fundamental, clinical, and surgical bases based on scientific evidence and good health practices and can be used in the professional training of nurses and in advanced nursing practice in cardiac surgery. Finally, it contributes to research, given its replicability, and guides the development of new research perspectives by detecting research methods used in each area.
CONTRIBUTIONS
Andrade MCCS contributed to the design of the study, as a double-blind researcher in the scoping review, analysis and discussion of the data and writing of the manuscript. Silveira IA participated as a double-blind researcher in the scope review. Tinoco JMVP contributed to writing the manuscript and critically reviewing the content. Cavalcanti ACD participated in the conception of the study, critical revision of the content and approval of the final version.
CONFLICTS OF INTERESTS
Nothing to report.
REFERENCES
- Précoma DB, Oliveira GMM, Simão AF, Dutra OP, Coelho-Filho OR, Izar MCO, et Updated Cardiovascular Prevention Guideline of the Brazilian Society of Cardiology - 2019. Arq Bras Cardiol.2019;113(4):787-891; doi: https://doi.org/10.5935/abc.20190204.
- D’Agostino RS, Jacobs JP, Badhwar V, Fernandez FG, Paone G, Wormuth DW, et al. The Society of Thoracic Surgeons Adult Cardiac Surgery Database: 2019. Update on Outcomes and Quality. Ann Thorac Surg. 2019;107(1):24–32. doi: https://org/10.1016/j.athoracsur.2018.10.004.
- Conselho Federal de Enfermagem. Diretrizes para elaboração de protocolos de enfermagem na atenção primária à saúde pelos Conselhos Regionais [Internet]. COFEN; 2018 [citado dez 2, 2020]. 22 p. Disponível: http://www.cofen.gov.br/wp-content/uploads/2019/03/Diretrizes-para-elabora%C3%A7%C3%A3o-de-protocolos-de-Enfermagem-.pdf
- Menezes HF, Camacho ACLF, Nóbrega MML, Fuly PSC, Fernandes SF, Silva RAR. Paths taken by Brazilian Nursing for the development of terminological subsets. Rev Lat Am Enfermagem. 2020; 28:e3270. doi: https://doi.org/10.1590/1518-8345.3132.3270.
- Andrade AYT, Tanaka PSL, Poveda VDB, Turrini RNT. Complicações no pós-operatório imediato de revascularização do miocárdio. Rev SOBECC. 2019;24(4):224–30. doi: https://doi.org/10.5327/Z1414-4425201900040008.
- Carmo TG, Santana RF, Lopes MVO, Nunes MM, Diniz CM, Rabelo-Silva ER, et al. Prognostic Indicators of Delayed Surgical Recovery in Patients Undergoing Cardiac Surgery. J Nurs Scholarsh. jul 2021; 53(4):428–38. doi: https://doi.org/10.1111/jnu.12662.
- Batistini HC, Sant’Anna ALGG, Giovanazzi RSD, Freitas VR, Costa SACM, Machado RC. Checklist validation for care provided to patients in the immediate postoperative period of cardiac surgery. J Clin Nurs. 2020;29(21–22):4171–9. doi: https://doi.org/10.1111/jocn.15446.
- Bolling K, Long T, Jennings CD, Dane FC, Carter KF. Bras for Breast Support After Sternotomy: Patient Satisfaction and Wear Compliance. Am J Crit Care. 2021;30(1):21–6. doi: https://doi.org/10.4037/ajcc2021687.
- Malheiro IC, Carmo TG, Cavalcanti ACD, Flores PVP. Intervenções de enfermagem no pós-operatório de cirurgia cardíaca. Res Soc Dev. 2020;9(7):e277974080. doi: http://dx.doi.org/10.33448/rsd-v9i7.4080.
- Peters M, Godfrey C, McInerney P, Munn Z, Trico A, Khalil H. Chapter 11: Scoping Reviews. Em: Aromataris E, Munn Z, organizadores. JBI Manual for Evidence Synthesis [Internet]. JBI; 2020 [cited abr 18, 2022]. Avaliable: https://wiki.jbi.global/display/MANUAL/Chapter+11%3A+Scoping+reviews
- Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169(7):467–73. doi: https://org/10.7326/M18-0850.
- Andrade M. Nursing care protocol for adult patients in immediate postoperative period of cardiac surgery: a scope review protocol. Figshare; 2021. doi: https://org/10.6084/m9.figshare.14787807.
- Andrade MCCS. Nursing care protocol for adult patients in immediate postoperative period of cardiac surgery: a scope review protocol. OSF; 2021. doi: https://doi.org/10.17605/OSF.IO/KHSMD.
- Younas A, Ali P. Five tips for developing useful literature summary tables for writing review articles. Evid Based Nurs. 2021;24(2):32–4. doi: http://dx.doi.org/10.1136/ebnurs-2021-103417.
- Herdman TH, Kamitsuru S, Lopes CT. NANDA international. Nursing Diagnoses: definitions and classifications (2021-2023). 12 ed. New York, NY: Thieme Medical Publishers; 2021.
- Bulechek GM, Dochterman JM, Wagner CM. Classificação das intervenções de enfermagem: NIC. 6 ed. Rio de Janeiro: Elsevier; 2016.
- Moorhead S, Johnson M, Mass ML, Swanson E. Classificação dos resultados de enfermagem: mensuração dos resultados em saúde. 5 ed. Rio de Janeiro: Elsevier; 2016.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. 2021;372:n71. doi: https://doi.org/10.1136/bmj.n71.
- Galdeano LE, Rossi LA, Santos CB, Dantas RAS. Diagnósticos de enfermagem no perioperatório de cirurgia cardíaca. Rev esc enferm. USP. 2006;40(1):26-33. doi: https://doi.org/10.1590/S0080-62342006000100004.
- Feuchtinger J, Halfens R, Dassen T. Pressure ulcer risk assessment immediately after cardiac surgery ? does it make a difference? A comparison of three pressure ulcer risk assessment instruments within a cardiac surgery population. Nurs Crit Care. 2007;12(1):42–9. Doi: https://doi.org/10.1111/j.1478-5153.2006.00198.x.
- Bickert AT, Gallagher C, Reiner A, Hager WJ, Stecker MM. Nursing Neurologic Assessments After Cardiac Operations. Ann Thorac Surg. 2008;85(2):554–60. doi: https://doi.org/10.1016/j.athoracsur.2007.09.050.
- Marmo L, Fowler S. Pain Assessment Tool in the Critically Ill Post–Open Heart Surgery Patient Population. Pain Manag Nurs. 2010;11(3):134–40. doi: https://doi.org/10.1016/j.pmn.2009.05.007.
- Guimarães RCM, Rabelo ER, Moraes MA, Azzolin K. Severity of postoperative cardiac surgery patients: an evolution analysis according to TISS-28. Rev Lat Am Enfermagem. 2010;18(1):61–6. doi: https://doi.org/10.1590/S0104-11692010000100010.
- Exarchopoulos T, Charitidou E, Dedeilias P, Charitos C, Routsi C. Scoring Systems for Outcome Prediction in a Cardiac Surgical Intensive Care Unit: A Comparative Study. Am J Crit Care. 2015;24(4):327–34. doi: http://dx.doi.org/10.4037/ajcc2015500.
- Fontes de Lara B, Nogueira PC, Poveda VDB. Diagnósticos de enfermagem no pós-operatório imediato de cirurgia de troca de válvula. Rev Enferm UFSM. 2017;7(4):700. doi: https://doi.org/10.5902/2179769225716.
- Santos ER, Lopes CT, Maria VLR, Barros ALBL. Risk factors for decreased cardiac output after coronary artery bypass grafting: a prospective cohort study. Eur J Cardiovasc Nurs. 2017;16(4):352–9. doi: https://doi.org/10.1177/1474515116681373.
- Rabelo-Silva ER, Cavalcanti ACD, Caldas MCRG, Lucena AF, Almeida MA, Linch GFC, et al. Advanced Nursing Process quality: Comparing the International Classification for Nursing Practice (ICNP) with the NANDA-International (NANDA-I) and Nursing Interventions Classification (NIC). J Clin Nurs. 2017;26(3–4):379–87. doi: https://doi.org/10.1111/jocn.13387.
- Fernandes RA, Silva JA. Cuidados de Enfermagem em pacientes no pós-operatório imediato (POI) de troca de válvula mitral: elaboração de um protocolo de atendimento. Rev UNINGÁ Review [internet]. 2011 [citado 18 abr 2022];8(1):61–71. Disponível: http://revista.uninga.br/index.php/uningareviews/article/view/565/221.
- Pivoto FL, Lunardi Filho WD, Santos SSC, Almeida MA, Silveira RS. Diagnósticos de enfermagem em pacientes no período pós-operatório de cirurgias cardíacas. Acta Paul Enferm. 2010;23(5):665–70. doi: https://doi.org/10.1590/S0103-21002010000500013.
- Hardin SR, Kaplow R. Cardiac surgery essentials for critical care nursing. 3th ed. American Association of Critical-care Nursing. Jones & Bartlett Learning: Burlington, MA; 2020.
- Lomivorotov VV, Efremov SM, Kirov MY, Fominskiy EV, Karaskov AM. Low-Cardiac-Output Syndrome After Cardiac Surgery. J Cardiothorac Vasc Anesth. 2017;31(1):291-308. doi: https://org/10.1053/j.jvca.2016.05.029.
- Duncan AE, Kartashov A, Robinson SB, Randall D, Zhang K, Luber J, et al. Risk factors, resource use, and cost of postoperative low cardiac output syndrome. J Thorac Cardiovasc Surg. 2022;163(5):1890-1898.e10. doi: https://doi.org/10.1016/j.jtcvs.2020.06.125.
- Kochar A, Zheng Y, Van Diepen S, Mehta RH, Westerhout CM, Mazer DC, et al. Predictors and associated clinical outcomes of low cardiac output syndrome following cardiac surgery: insights from the LEVO-CTS trial. Eur Heart J Acute Cardiovasc Care. 2022;11(11):818-825. doi: https://doi.org/10.1093/ehjacc/zuac114.
- Pérez Vela JL, Jiménez Rivera JJ, Alcalá Llorente MÁ, González de Marcos B, Torrado H, García Laborda C, et al. Low cardiac output syndrome in the postoperative period of cardiac surgery. Profile, differences in clinical course and prognosis. The ESBAGA study. Med Intensiva. 2018;42(3):159-167. doi: https://doi.org/10.1016/j.medin.2017.05.009.
- Bowdish ME, D'Agostino RS, Thourani VH, Schwann TA, Krohn C, Desai N, et al. STS Adult Cardiac Surgery Database: 2021 Update on Outcomes, Quality, and Research. Ann Thorac Surg. 2021;111(6):1770-1780. doi: https://org/10.1016/j.athoracsur.2021.03.043.
- Vesteinsdottir E, Helgason KO, Sverrisson KO, Gudlaugsson O, Karason S. Infections and outcomes after cardiac surgery—The impact of outbreaks traced to transesophageal echocardiography probes. Acta Anaesthesiol Scand. 2019;aas.13360. doi: https://doi.org/10.1111/aas.13360.
- Tse L, Bowering JB, Schwarz SK, Moore RL, Sztramko R, Barr AM. Incidence and risk factors for impaired mobility in older cardiac surgery patients during the early postoperative period. Geriatr Gerontol Int. 2015;15(3):276-81. doi: https://doi.org/10.1111/ggi.12269.
- Hamadé DCE, Moraes CS, Costa CCP, Martins MOD. Nursing diagnoses with coronary patients in the light of Calista Roy's theory. pesq.: cuid. fundam. online. 2020;12:129-136. doi: https://doi.org/10.9789/2175-5361.rpcfo.v12.7137.
- Holanda da Cunha G, Lima AK, Maia AM, Correia MA, Barbosa K, Rodrigues de Oliveira RC. Diagnósticos de enfermagem segundo a teoria do autocuidado em pacientes com infarto do miocárdio. 2018;18(2):222-233. doi: https://doi.org/10.5294/aqui.2018.18.2.9.
- Doiron KA, Hoffmann TC, Beller EM. Early intervention (mobilization or active exercise) for critically ill adults in the intensive care unit. Cochrane Database Syst Rev. 2018;3(3):CD010754. doi: https://doi.org/10.1002/14651858.CD010754.pub2.
- Padua BLR, Tinoco JMVP, Dias BF, Carmo TG, Flores PVP, Cavalcanti ACD. Cross-mapping of nursing diagnoses and interventions in decompensated heart failure. Rev Gaúcha Enferm. 2022;43. doi: https://doi.org/10.1590/1983-1447.2022.20200400.en.
- Kanji S, MacPhee H, Singh A, Johanson C, Fairbairn J, Lloyd T, et al. Validation of the Critical Care Pain Observation Tool in Critically Ill Patients With Delirium: A Prospective Cohort Study. Crit Care Med. 2016;44(5):943–7. doi: https://doi.org/10.1097/CCM.0000000000001522.
- Chookalayi H, Heidarzadeh M, Hasanpour M, Jabrailzadeh S, Sadeghpour F. A Study on The Psychometric Properties of Revised-Nonverbal Pain Scale and Original-Nonverbal Pain Scale in Iranian Nonverbal-Ventilated Patients. Indian J Crit Care Med. 2017;21(7):429–35. doi: https://doi.org/10.4103/ijccm.IJCCM_114_17.
- Gélinas C, Joffe AM, Szumita PM, Payen JF, Bérubé M, Shahiri TS, et al. A Psychometric Analysis Update of Behavioral Pain Assessment Tools for Noncommunicative, Critically Ill Adults. AACN Adv Crit Care. 2019;30(4):365–87. Doi: https://org/10.4037/aacnacc2019952.
- Baker S, Beauchamp K, Ballinghoff J, Escherich A, Cheung AT, Stecker MM. Utility of the neurologic intensive care evaluation (NICE) in detecting neurologic deficit after cardiac operations--a pilot study [Internet]. Med Sci Monit Int Med J Exp Clin Res. 2003 [Cited jan 05, 2023];9(5):CR151-156. Avaliable: https://pubmed.ncbi.nlm.nih.gov/12761449/.
- Singh N, Gimpel D, Parkinson G, Conaglen P, Meikle F, Lin Z, et al. Assessment of the EuroSCORE II in a New Zealand Tertiary Centre. Heart Lung Circ. 2019;28(11):1670–6. doi: https://doi.org/10.1016/j.hlc.2018.09.004.
- Pivatto Junior F, Bellagamba CCA, Pianca EG, Fernandes FS, Butzke M, Busato SB, et al. Analysis of Risk Scores to Predict Mortality in Patients Undergoing Cardiac Surgery for Endocarditis. Arquivos Brasileiros de Cardiologia. 2020;114(3):518-524. doi: https://org/10.36660/abc.20190050.
- Wang ZW, Zheng J, You LM, Wang YX, Gao MR, Guan XD. Evaluation of the simplified therapeutic intervention scoring system: Chinese version. Intensive Crit Care Nurs. 2018;45:85–90. doi: https://doi.org/10.1016/j.iccn.2017.09.009.
Correspondence:
Maryanna Cruz da Costa e Silva Andrade
E-mail: maryannasilva@id.uff.br
Copyright© 2024 Revista de Enfermagem UFPE on line/REUOL.
Este é um artigo de acesso aberto distribuído sob a Atribuição CC BY 4.0 Creative Commons Attribution-ShareAlike 4.0 International License, a qual permite que outros distribuam, remixem, adaptem e criem a partir do seu trabalho, mesmo para fins comerciais, desde que lhe atribuam o devido crédito pela criação original. É recomendada para maximizar a disseminação e uso dos materiais licenciados.





















